Diastat: Package Insert / Prescribing Info
Package insert / product label
Generic name: diazepam
Dosage form: rectal gel
Drug class: Benzodiazepine anticonvulsants
Medically reviewed by Drugs.com. Last updated on Jan 4, 2024.
On This Page
WARNING: RISKS FROM CONCOMITANT USE WITH OPIOIDS; ABUSE, MISUSE, AND ADDICTION; and DEPENDENCE AND WITHDRAWAL REACTIONS
- Concomitant use of benzodiazepines and opioids may result in profound sedation, respiratory depression, coma, and death. Reserve concomitant prescribing of these drugs for patients for whom alternative treatment options are inadequate. Limit dosages and durations to the minimum required. Follow patients for signs and symptoms of respiratory depression and sedation (seeWARNINGSand PRECAUTIONS).
- The use of benzodiazepines, including DIASTAT, exposes users to risks of abuse, misuse, and addiction, which can lead to overdose or death. Abuse and misuse of benzodiazepines commonly involve concomitant use of other medications, alcohol, and/or illicit substances, which is associated with an increased frequency of serious adverse outcomes. Before prescribing DIASTAT and throughout treatment, assess each patient’s risk for abuse, misuse, and addiction (seeWARNINGS).
- The continued use of benzodiazepines may lead to clinically significant physical dependence. The risks of dependence and withdrawal increase with longer treatment duration and higher daily dose. Although DIASTAT is indicated only for intermittent use (see INDICATIONS AND USAGEand DOSAGE AND ADMINISTRATION), if used more frequently than recommended, abrupt discontinuation or rapid dosage reduction of DIASTAT may precipitate acute withdrawal reactions, which can be life-threatening. For patients using DIASTAT more frequently than recommended, to reduce the risk of withdrawal reactions, use a gradual taper to discontinue DIASTAT (see WARNINGS).
Diastat Description
Diazepam rectal gel rectal delivery system is a non-sterile diazepam gel provided in a prefilled, unit-dose, rectal delivery system. Diazepam rectal gel contains 5 mg/mL diazepam, benzoic acid, benzyl alcohol (1.5%), ethyl alcohol (10%), hydroxypropyl methylcellulose, propylene glycol, purified water, and sodium benzoate. Diazepam rectal gel is clear to slightly yellow and has a pH between 6.5-7.5.
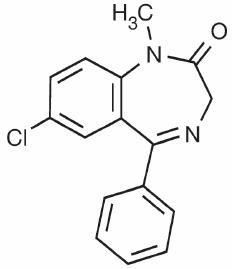
Diazepam, the active ingredient of diazepam rectal gel, is a benzodiazepine anticonvulsant with the chemical name 7-chloro-1,3-dihydro-1-methyl-5-phenyl-2 H-1,4-benzodiazepin-2-one. The structural formula is as follows:
Diastat - Clinical Pharmacology
Mechanism of Action
Although the precise mechanism by which diazepam exerts its antiseizure effects is unknown, animal and in vitro studies suggest that diazepam acts to suppress seizures through an interaction with γ-aminobutyric acid (GABA) receptors of the A-type (GABA A). GABA, the major inhibitory neurotransmitter in the central nervous system (CNS), acts at this receptor to open the membrane channel allowing chloride ions to flow into neurons. Entry of chloride ions causes an inhibitory potential that reduces the ability of neurons to depolarize to the threshold potential necessary to produce action potentials. Excessive depolarization of neurons is implicated in the generation and spread of seizures. It is believed that diazepam enhances the actions of GABA by causing GABA to bind more tightly to the GABA Areceptor.
Pharmacokinetics
Pharmacokinetic information of diazepam following rectal administration was obtained from studies conducted in healthy adult subjects. No pharmacokinetic studies were conducted in pediatric patients. Therefore, information from the literature is used to define pharmacokinetic labeling in the pediatric population.
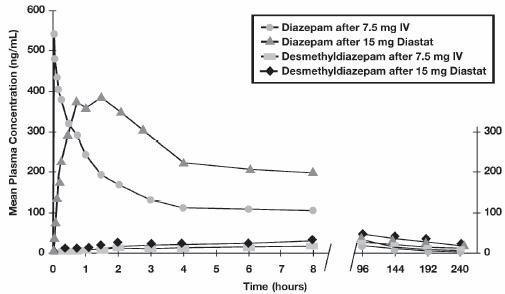
Diazepam rectal gel is well absorbed following rectal administration, reaching peak plasma concentrations in 1.5 hours. The absolute bioavailability of diazepam rectal gel relative to Valium injectable is 90%. The volume of distribution of diazepam rectal gel is calculated to be approximately 1 L/kg. The mean elimination half-life of diazepam and desmethyldiazepam following administration of a 15 mg dose of diazepam rectal gel was found to be about 46 hours (CV=43%) and 71 hours (CV=37%), respectively.
Both diazepam and its major active metabolite desmethyldiazepam bind extensively to plasma proteins (95-98%).
Metabolism and Elimination:It has been reported in the literature that diazepam is extensively metabolized to one major active metabolite (desmethyldiazepam) and two minor active metabolites, 3-hydroxydiazepam (temazepam) and 3-hydroxy-N-diazepam (oxazepam) in plasma. At therapeutic doses, desmethyldiazepam is found in plasma at concentrations equivalent to those of diazepam while oxazepam and temazepam are not usually detectable. The metabolism of diazepam is primarily hepatic and involves demethylation (involving primarily CYP2C19 and CYP3A4) and 3-hydroxylation (involving primarily CYP3A4), followed by glucuronidation. The marked inter-individual variability in the clearance of diazepam reported in the literature is probably attributable to variability of CYP2C19 (which is known to exhibit genetic polymorphism; about 3-5% of Caucasians have little or no activity and are “poor metabolizers”) and CYP3A4. No inhibition was demonstrated in the presence of inhibitors selective for CYP2A6, CYP2C9, CYP2D6, CYP2E1, or CYP1A2, indicating that these enzymes are not significantly involved in metabolism of diazepam.
Special Populations
Hepatic Impairment:
No pharmacokinetic studies were conducted with diazepam rectal gel in hepatically impaired subjects. Literature review indicates that following administration of 0.1 to 0.15 mg/kg of diazepam intravenously, the half-life of diazepam was prolonged by two to five-fold in subjects with alcoholic cirrhosis (n=24) compared to age-matched control subjects (n=37) with a corresponding decrease in clearance by half: however, the exact degree of hepatic impairment in these subjects was not characterized in this literature (see PRECAUTIONS).
Renal Impairment:
The pharmacokinetics of diazepam have not been studied in renally impaired subjects (see PRECAUTIONS).
Pediatrics:
No pharmacokinetic studies were conducted with diazepam rectal gel in the pediatric population. However, literature review indicates that following IV administration (0.33 mg/kg), diazepam has a longer half-life in neonates (birth up to one month; approximately 50-95 hours) and infants (one month up to two years; about 40-50 hours), whereas it has a shorter half-life in children (two to 12 years; approximately 15-21 hours) and adolescents (12 to 16 years; about 18-20 hours) (see PRECAUTIONS).
Elderly:
A study of single dose IV administration of diazepam (0.1 mg/kg) indicates that the elimination half-life of diazepam increases linearly with age, ranging from about 15 hours at 18 years (healthy young adults) to about 100 hours at 95 years (healthy elderly) with a corresponding decrease in clearance of free diazepam (see PRECAUTIONSand DOSAGE AND ADMINISTRATION).
Effect of Gender, Race, and Cigarette Smoking:
No targeted pharmacokinetic studies have been conducted to evaluate the effect of gender, race, and cigarette smoking on the pharmacokinetics of diazepam. However, covariate analysis of a population of treated patients following administration of diazepam rectal gel, indicated that neither gender nor cigarette smoking had any effect on the pharmacokinetics of diazepam.
Clinical Studies
The effectiveness of diazepam rectal gel has been established in two adequate and well controlled clinical studies in children and adults exhibiting the seizure pattern described below under INDICATIONS AND USAGE.
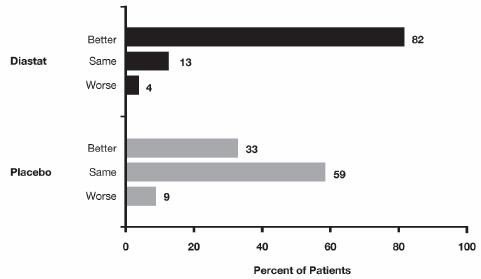
A randomized, double-blind study compared sequential doses of diazepam rectal gel and placebo in 91 patients (47 children, 44 adults) exhibiting the appropriate seizure profile. The first dose was given at the onset of an identified episode. Children were dosed again four hours after the first dose and were observed for a total of 12 hours. Adults were dosed at four and 12 hours after the first dose and were observed for a total of 24 hours. Primary outcomes for this study were seizure frequency during the period of observation and a global assessment that took into account the severity and nature of the seizures as well as their frequency.
The median seizure frequency for the diazepam rectal gel treated group was zero seizures per hour, compared to a median seizure frequency of 0.3 seizures per hour for the placebo group, a difference that was statistically significant (p <0.0001). All three categories of the global assessment (seizure frequency, seizure severity, and “overall”) were also found to be statistically significant in favor of diazepam rectal gel (p < 0.0001). The following histogram displays the results for the “overall” category of the global assessment.
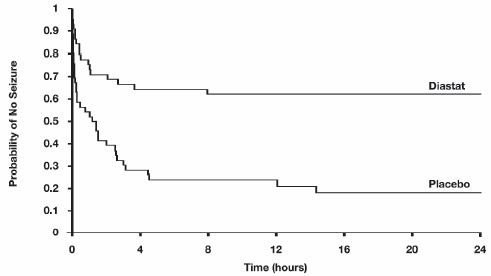
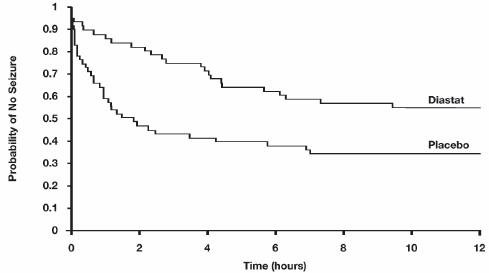
Patients treated with diazepam rectal gel experienced prolonged time-to-next-seizure compared to placebo (p = 0.0002) as shown in the following graph.
In addition, 62% of patients treated with diazepam rectal gel were seizure-free during the observation period compared to 20% of placebo patients.
Analysis of response by gender and age revealed no substantial differences between treatment in either of these subgroups. Analysis of response by race was considered unreliable, due to the small percentage of non-Caucasians.
A second double-blind study compared single doses of diazepam rectal gel and placebo in 114 patients (53 children, 61 adults). The dose was given at the onset of the identified episode and patients were observed for a total of 12 hours. The primary outcome in this study was seizure frequency. The median seizure frequency for the diazepam rectal gel-treated group was zero seizures per 12 hours, compared to a median seizure frequency of 2.0 seizures per 12 hours for the placebo group, a difference that was statistically significant (p < 0.03). Patients treated with diazepam rectal gel experienced prolonged time-to-next-seizure compared to placebo (p = 0.0072) as shown in the following graph.
In addition, 55% of patients treated with diazepam rectal gel were seizure-free during the observation period compared to 34% of patients receiving placebo. Overall, caregivers judged diazepam rectal gel to be more effective than placebo (p = 0.018), based on a 10 centimeter visual analog scale. In addition, investigators also evaluated the effectiveness of diazepam rectal gel and judged diazepam rectal gel to be more effective than placebo (p < 0.001).
An analysis of response by gender revealed a statistically significant difference between treatments in females but not in males in this study, and the difference between the 2 genders in response to the treatments reached borderline statistical significance. Analysis of response by race was considered unreliable, due to the small percentage of non-Caucasians.
Indications and Usage for Diastat
Diazepam rectal gel is intended for the acute treatment of intermittent, stereotypic episodes of frequent seizure activity (i.e., seizure clusters, acute repetitive seizures) that are distinct from a patient’s usual seizure pattern in patients with epilepsy 2 years of age and older.
Contraindications
Diazepam rectal gel is contraindicated in patients with a known hypersensitivity to diazepam. Diazepam rectal gel may be used in patients with open angle glaucoma who are receiving appropriate therapy but is contraindicated in acute narrow angle glaucoma.
Warnings
General
Diazepam rectal gel should only be administered by caregivers who in the opinion of the prescribing physician 1) are able to distinguish the distinct cluster of seizures (and/or the events presumed to herald their onset) from the patient’s ordinary seizure activity, 2) have been instructed and judged to be competent to administer the treatment rectally, 3) understand explicitly which seizure manifestations may or may not be treated with diazepam rectal gel, and 4) are able to monitor the clinical response and recognize when that response is such that immediate professional medical evaluation is required.
Risks from Concomitant Use with Opioids
Concomitant use of benzodiazepines, including DIASTAT and DIASTAT ACUDIAL, and opioids may result in profound sedation, respiratory depression, coma, and death. Because of these risks, reserve concomitant prescribing of benzodiazepines and opioids for patients for whom alternative treatment options are inadequate.
Observational studies have demonstrated that concomitant use of opioid analgesics and benzodiazepines increases the risk of drug-related mortality compared to use of opioids alone. If a decision is made to prescribe DIASTAT or DIASTAT ACUDIAL concomitantly with opioids, prescribe the lowest effective dosages and minimum durations of concomitant use, and follow patients closely for signs and symptoms of respiratory depression and sedation. Advise both patients and caregivers about the risks of respiratory depression and sedation when DIASTAT or DIASTAT ACUDIAL is used with opioids (see PRECAUTIONS).
Abuse, Misuse, and Addiction
The use of benzodiazepines, including DIASTAT, exposes users to the risks of abuse, misuse, and addiction, which can lead to overdose or death. Abuse and misuse of benzodiazepines often (but not always) involve the use of doses greater than the maximum recommended dosage and commonly involve concomitant use of other medications, alcohol, and/or illicit substances, which is associated with an increased frequency of serious adverse outcomes, including respiratory depression, overdose, or death (see DRUG ABUSE AND DEPENDENCE: Abuse).
Before prescribing DIASTAT and throughout treatment, assess each patient’s risk for abuse, misuse, and addiction. Use of DIASTAT, particularly in patients at elevated risk, necessitates counseling about the risks and proper use of DIASTAT along with monitoring for signs and symptoms of abuse, misuse, and addiction. Do not exceed the recommended dosing frequency; avoid or minimize concomitant use of CNS depressants and other substances associated with abuse, misuse, and addiction (e.g., opioid analgesics, stimulants); and advise patients on the proper disposal of unused drug. If a substance use disorder is suspected, evaluate the patient and institute (or refer them for) early treatment, as appropriate.
Dependence and Withdrawal Reactions After Use of DIASTAT More Frequently Than Recommended
For patients using DIASTAT more frequently than recommended, to reduce the risk of withdrawal reactions, use a gradual taper to discontinue DIASTAT (a patient-specific plan should be used to taper the dose).
Patients at an increased risk of withdrawal adverse reactions after benzodiazepine discontinuation or rapid dosage reduction include those who take higher dosages, and those who have had longer durations of use.
Acute Withdrawal Reactions
The continued use of benzodiazepines may lead to clinically significant physical dependence. Although DIASTAT is indicated only for intermittent use (see INDICATIONS AND USAGEand DOSAGE AND ADMINISTRATION), if used more frequently than recommended, abrupt discontinuation or rapid dosage reduction of DIASTAT, or administration of flumazenil (a benzodiazepine antagonist) may precipitate acute withdrawal reactions, which can be life-threatening (e.g., seizures) (see DRUG ABUSE AND DEPENDENCE: Dependence) .
Protracted Withdrawal Syndrome
In some cases, benzodiazepine users have developed a protracted withdrawal syndrome with withdrawal symptoms lasting weeks to more than 12 months (see DRUG ABUSE AND DEPENDENCE: Dependence).
CNS Depression
Because diazepam rectal gel produces CNS depression, patients receiving this drug who are otherwise capable and qualified to do so should be cautioned against engaging in hazardous occupations requiring mental alertness, such as operating machinery, driving a motor vehicle, or riding a bicycle until they have completely returned to their level of baseline functioning.
Although diazepam rectal gel is indicated for use solely on an intermittent basis, the potential for a synergistic CNS-depressant effect when used simultaneously with alcohol or other CNS depressants must be considered by the prescribing physician, and appropriate recommendations made to the patient and/or caregiver.
Prolonged CNS depression has been observed in neonates treated with diazepam. Therefore, diazepam rectal gel is not recommended for use in children under six months of age.
Neonatal Sedation and Withdrawal Syndrome
Use of DIASTAT late in pregnancy can result in sedation (respiratory depression, lethargy, hypotonia) and/or withdrawal symptoms (hyperreflexia, irritability, restlessness, tremors, inconsolable crying, and feeding difficulties) in the neonate (seePRECAUTIONS: Pregnancy). Monitor neonates exposed to DIASTAT during pregnancy or labor for signs of sedation and monitor neonates exposed to DIASTAT during pregnancy for signs of withdrawal; manage these neonates accordingly.
Chronic Use
Diazepam rectal gel is not recommended for chronic, daily use as an anticonvulsant because of the potential for development of tolerance to diazepam. Chronic daily use of diazepam may increase the frequency and/or severity of tonic clonic seizures, requiring an increase in the dosage of standard anticonvulsant medication. In such cases, abrupt withdrawal of chronic diazepam may also be associated with a temporary increase in the frequency and/or severity of seizures.
Precautions
Information for Patients
Risks from Concomitant Use with Opioids:
Inform patients and caregivers that potentially fatal additive effects may occur if DIASTAT or DIASTAT ACUDIAL is used with opioids and not to use such drugs concomitantly unless supervised by a health care provider (see WARNINGSand PRECAUTIONS: Drug Interactions).
Abuse, Misuse, and Addiction:Inform patients that the use of DIASTAT more frequently than recommended, even at recommended dosages, exposes users to risks of abuse, misuse, and addiction, which can lead to overdose and death, especially when used in combination with other medications (e.g., opioid analgesics), alcohol, and/or illicit substances. Inform patients about the signs and symptoms of benzodiazepine abuse, misuse, and addiction; to seek medical help if they develop these signs and/or symptoms; and on the proper disposal of unused drug (see WARNINGS: Abuse, Misuse, and Addictionand DRUG ABUSE AND DEPENDENCE) .
Withdrawal Reactions:Inform patients that use of DIASTAT more frequently than recommended may lead to clinically significant physical dependence and that abrupt discontinuation or rapid dosage reduction of DIASTAT may precipitate acute withdrawal reactions, which can be life-threatening. Inform patients that in some cases, patients taking benzodiazepines have developed a protracted withdrawal syndrome with withdrawal symptoms lasting weeks to more than 12 months (see WARNINGS: Dependence and Withdrawal Reactionsand DRUG ABUSE AND DEPENDENCE) .
Administration:Prescribers are strongly advised to take all reasonable steps to ensure that caregivers fully understand their role and obligations vis a vis the administration of diazepam rectal gel to individuals in their care. Prescribers should routinely discuss the steps in the Patient/Caregiver Package Insert (see Patient/Caregiver Insert printed at the end of the product labeling and also included in the product carton). The successful and safe use of diazepam rectal gel depends in large measure on the competence and performance of the caregiver.
Prescribers should advise caregivers that they expect to be informed immediately if a patient develops any new findings which are not typical of the patient’s characteristic seizure episode.
Interference With Cognitive and Motor Performance:Because benzodiazepines have the potential to impair judgment, thinking, or motor skills, patients should be cautioned about operating hazardous machinery, including automobiles, until they are reasonably certain that diazepam rectal gel therapy does not affect them adversely.
Pregnancy
Advise pregnant females that use of DIASTAT late in pregnancy can result in sedation (respiratory depression, lethargy, hypotonia) and/or withdrawal symptoms (hyperreflexia, irritability, restlessness, tremors, inconsolable crying, and feeding difficulties) in newborns (see WARNINGS: Neonatal Sedation and Withdrawal Syndromeand PRECAUTIONS: Pregnancy). Instruct patients to inform their healthcare provider if they are pregnant.
Encourage patients to enroll in the North American Antiepileptic Drug (NAAED) Pregnancy Registry if they become pregnant while taking DIASTAT. The registry is collecting information about the safety of antiepileptic drugs during pregnancy (seePRECAUTIONS: Pregnancy).
Lactation
Counsel patients that diazepam, the active ingredient in DIASTAT, is present in breast milk. Instruct patients to inform their healthcare provider if they are breastfeeding or plan to breastfeed. Instruct breastfeeding patients who take DIASTAT to monitor their infants for excessive sedation, poor feeding and poor weight gain, and to seek medical attention if they notice these signs (seePRECAUTIONS: Nursing Mothers) .
Concomitant Medication
Although diazepam rectal gel is indicated for use solely on an intermittent basis, the potential for a synergistic CNS-depressant effect when used simultaneously with alcohol or other CNS-depressants must be considered by the prescribing physician, and appropriate recommendations made to the patient and/or caregiver.
Drug Interactions
There have been no clinical studies or reports in literature to evaluate the interaction of rectally administered diazepam with other drugs. As with all drugs, the potential for interaction by a variety of mechanisms is a possibility.
Effect of Concomitant Use of Benzodiazepines and Opioids:The concomitant use of benzodiazepines and opioids increases the risk of respiratory depression because of actions at different receptor sites in the CNS that control respiration. Benzodiazepines interact at GABA Asites, and opioids interact primarily at mu receptors. When benzodiazepines and opioids are combined, the potential for benzodiazepines to significantly worsen opioid-related respiratory depression exists. Limit dosage and duration of concomitant use of benzodiazepines and opioids, and follow patients closely for respiratory depression and sedation.
Other Psychotropic Agents or Other CNS Depressants:If diazepam rectal gel is to be combined with other psychotropic agents or other CNS depressants, careful consideration should be given to the pharmacology of the agents to be employed particularly with known compounds which may potentiate the action of diazepam, such as phenothiazines, narcotics, barbiturates, MAO inhibitors and other antidepressants.
Cimetidine:The clearance of diazepam and certain other benzodiazepines can be delayed in association with cimetidine administration. The clinical significance of this is unclear.
Valproate:Valproate may potentiate the CNS-depressant effects of diazepam.
Effect of Other Drugs on Diazepam Metabolism:In vitro studies using human liver preparations suggest that CYP2C19 and CYP3A4 are the principal isozymes involved in the initial oxidative metabolism of diazepam. Therefore, potential interactions may occur when diazepam is given concurrently with agents that affect CYP2C19 and CYP3A4 activity. Potential inhibitors of CYP2C19 (e.g., cimetidine, quinidine, and tranylcypromine) and CYP3A4 (e.g., ketoconazole, troleandomycin, and clotrimazole) could decrease the rate of diazepam elimination, while inducers of CYP2C19 (e.g., rifampin) and CYP3A4 (e.g., carbamazepine, phenytoin, dexamethasone, and phenobarbital) could increase the rate of elimination of diazepam.
Effect of Diazepam on the Metabolism of Other Drugs:There are no reports as to which isozymes could be inhibited or induced by diazepam. But, based on the fact that diazepam is a substrate for CYP2C19 and CYP3A4, it is possible that diazepam may interfere with the metabolism of drugs which are substrates for CYP2C19, (e.g. omeprazole, propranolol, and imipramine) and CYP3A4 (e.g. cyclosporine, paclitaxel, terfenadine, theophylline, and warfarin) leading to a potential drug-drug interaction.
Carcinogenesis, Mutagenesis, Impairment of Fertility
The carcinogenic potential of rectal diazepam has not been evaluated. In studies in which mice and rats were administered diazepam in the diet at a dose of 75 mg/kg/day (approximately six and 12 times, respectively, the maximum recommended human dose [MRHD=1 mg/kg/day] on a mg/m 2basis) for 80 and 104 weeks, respectively, an increased incidence of liver tumors was observed in males of both species.
The data currently available are inadequate to determine the mutagenic potential of diazepam.
Reproduction studies in rats showed decreases in the number of pregnancies and in the number of surviving offspring following administration of an oral dose of 100 mg/kg/day (approximately 16 times the MRHD on a mg/m 2basis) prior to and during mating and throughout gestation and lactation. No adverse effects on fertility or offspring viability were noted at a dose of 80 mg/kg/day (approximately 13 times the MRHD on a mg/m 2basis).
Pregnancy
Pregnancy Exposure Registry
There is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to AEDs, such as DIASTAT, during pregnancy. Healthcare providers are encouraged to recommend that pregnant women taking DIASTATenroll in the NAAED Pregnancy Registry by calling 1-888-233-2334 or online at http://www.aedpregnancyregistry.org/.
Risk Summary
Neonates born to mothers using benzodiazepines late in pregnancy have been reported to experience symptoms of sedation and/or neonatal withdrawal (see WARNINGS: Neonatal Sedation and Withdrawal Syndromeand PRECAUTIONS: Pregnancy, Clinical Considerations). Available data from published observational studies of pregnant women exposed to benzodiazepines do not report a clear association with benzodiazepines and major birth defects (see Human Data).
In animal studies, administration of diazepam during the organogenesis period of pregnancy resulted in increased incidences of fetal malformations at doses greater than those used clinically. Data for diazepam and other benzodiazepines suggest the possibility of increased neuronal cell death and long-term effects on neurobehavioral and immunological function based on findings in animals following prenatal or early postnatal exposure at clinically relevant doses (see Animal Data).
The background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated risk of major birth defects and of miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Clinical Considerations
Fetal/Neonatal Adverse Reactions
Benzodiazepines cross the placenta and may produce respiratory depression, hypotonia, and sedation in neonates. Monitor neonates exposed to DIASTAT during pregnancy or labor for signs of sedation, respiratory depression, hypotonia, and feeding problems. Monitor neonates exposed to DIASTAT during pregnancy for signs of withdrawal. Manage these neonates accordingly (see WARNINGS: Neonatal Sedation and Withdrawal Syndrome).
Data
Human Data
Published data from observational studies on the use of benzodiazepines during pregnancy do not report a clear association with benzodiazepines and major birth defects. Although early studies reported an increased risk of congenital malformations with diazepam and chlordiazepoxide, there was no consistent pattern noted. In addition, the majority of more recent case-control and cohort studies of benzodiazepine use during pregnancy, which were adjusted for confounding exposures to alcohol, tobacco and other medications, have not confirmed these findings.
Animal Data
Diazepam has been shown to produce increased incidences of fetal malformations in mice and hamsters when given orally at single doses of 100 mg/kg or greater (approximately 20 times the maximum recommended adult human dose [0.4 mg/kg/day] or greater on a mg/m2 basis). Cleft palate and exencephaly are the most common and consistently reported malformations produced in these species by administration of high, maternally-toxic doses of diazepam during organogenesis. In published animal studies, administration of benzodiazepines or other drugs that enhance GABAergic neurotransmission to neonatal rats has been reported to result in widespread apoptotic neurodegeneration in the developing brain at plasma concentrations relevant for seizure control in humans. The window of vulnerability to these changes in rats (postnatal days 0-14) includes a period of brain development that takes place during the third trimester of pregnancy in humans.
Nursing Mothers
- Risk Summary
Diazepam is present in breastmilk. There are reports of sedation, poor feeding and poor weight gain in infants exposed to benzodiazepines through breast milk. There are no data on the effects of diazepam on milk production.
The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for DIASTAT and any potential adverse effects on the breastfed infant from DIASTAT or from the underlying maternal condition.
Clinical Considerations
Infants exposed to DIASTAT through breast milk should be monitored for sedation, poor feeding and poor weight gain. Because diazepam and its metabolites may be present in human breast milk for prolonged periods of time after acute use of diazepam rectal gel, patients should be advised not to breastfeed for an appropriate period of time after receiving treatment with diazepam rectal gel.
Caution in Renally Impaired Patients
Metabolites of diazepam rectal gel are excreted by the kidneys; to avoid their excess accumulation, caution should be exercised in the administration of the drug to patients with impaired renal function.
Caution in Hepatically Impaired Patients
Concomitant liver disease is known to decrease the clearance of diazepam (see CLINICAL PHARMACOLOGY: Special Populations, Hepatic Impairment). Therefore, diazepam rectal gel should be used with caution in patients with liver disease.
Use in Pediatrics
The controlled trials demonstrating the effectiveness of diazepam rectal gel included children two years of age and older. Clinical studies have not been conducted to establish the efficacy and safety of diazepam rectal gel in children under two years of age.
Use in Patients with Compromised Respiratory Function
Diazepam rectal gel should be used with caution in patients with compromised respiratory function related to a concurrent disease process (e.g., asthma, pneumonia) or neurologic damage.
Use in Elderly
In elderly patients diazepam rectal gel should be used with caution due to an increase in half-life with a corresponding decrease in the clearance of free diazepam. It is also recommended that the dosage be decreased to reduce the likelihood of ataxia or oversedation.
Adverse Reactions/Side Effects
Diazepam rectal gel adverse event data were collected from double-blind, placebo-controlled studies and open-label studies. The majority of adverse events were mild to moderate in severity and transient in nature.
Two patients who received diazepam rectal gel died seven to 15 weeks following treatment; neither of these deaths was deemed related to diazepam rectal gel.
The most frequent adverse event reported to be related to diazepam rectal gel in the two double-blind, placebo-controlled studies was somnolence (23%). Less frequent adverse events were dizziness, headache, pain, abdominal pain, nervousness, vasodilatation, diarrhea, ataxia, euphoria, incoordination, asthma, rhinitis, and rash, which occurred in approximately 2-5% of patients.
Approximately 1.4% of the 573 patients who received diazepam rectal gel in clinical trials of epilepsy discontinued treatment because of an adverse event. The adverse event most frequently associated with discontinuation (occurring in three patients) was somnolence. Other adverse events most commonly associated with discontinuation and occurring in two patients were hypoventilation and rash. Adverse events occurring in one patient were asthenia, hyperkinesia, incoordination, vasodilatation and urticaria. These events were judged to be related to diazepam rectal gel.
In the two domestic double-blind, placebo-controlled, parallel-group studies, the proportion of patients who discontinued treatment because of adverse events was 2% for the group treated with diazepam rectal gel, versus 2% for the placebo group. In the diazepam rectal gel group, the adverse events considered the primary reason for discontinuation were different in the two patients who discontinued treatment; one discontinued due to rash and one discontinued due to lethargy. The primary reason for discontinuation in the patients treated with placebo was lack of effect.
Adverse Event Incidence in Controlled Clinical Trials
Table 1 lists treatment-emergent signs and symptoms that occurred in > 1% of patients enrolled in parallel-group, placebo-controlled trials and were numerically more common in the diazepam rectal gel group. Adverse events were usually mild or moderate in intensity.
The prescriber should be aware that these figures, obtained when diazepam rectal gel was added to concurrent antiepileptic drug therapy, cannot be used to predict the frequency of adverse events in the course of usual medical practice when patient characteristics and other factors may differ from those prevailing during clinical studies. Similarly, the cited frequencies cannot be directly compared with figures obtained from other clinical investigations involving different treatments, uses, or investigators. An inspection of these frequencies, however, does provide the prescribing physician with one basis to estimate the relative contribution of drug and non-drug factors to the adverse event incidences in the population studied.
|
Body System |
COSTART
|
DIASTAT
|
Placebo
|
|
Body as a Whole |
Headache |
5% |
4% |
|
Cardiovascular |
Vasodilatation |
2% |
0% |
|
Digestive |
Diarrhea |
4% |
<1% |
|
Nervous |
Ataxia
|
3%
|
<1%
|
|
Respiratory |
Asthma |
2% |
0% |
|
Skin and Appendages |
Rash |
3% |
0% |
Other events reported by 1% or more of patients treated in controlled trials but equally or more frequent in the placebo group than in the diazepam rectal gel group were abdominal pain, pain, nervousness, and rhinitis. Other events reported by fewer than 1% of patients were infection, anorexia, vomiting, anemia, lymphadenopathy, grand mal convulsion, hyperkinesia, cough increased, pruritus, sweating, mydriasis, and urinary tract infection.
The pattern of adverse events was similar for different age, race and gender groups.
Other Adverse Events Observed During All Clinical Trials
Diazepam rectal gel has been administered to 573 patients with epilepsy during all clinical trials, only some of which were placebo-controlled. During these trials, all adverse events were recorded by the clinical investigators using terminology of their own choosing. To provide a meaningful estimate of the proportion of individuals having adverse events, similar types of events were grouped into a smaller number of standardized categories using modified COSTART dictionary terminology. These categories are used in the listing below. All of the events listed below occurred in at least 1% of the 573 individuals exposed to diazepam rectal gel.
All reported events are included except those already listed above, events unlikely to be drug-related, and those too general to be informative. Events are included without regard to determination of a causal relationship to diazepam.
BODY AS A WHOLE:Asthenia
CARDIOVASCULAR:Hypotension, vasodilatation
NERVOUS:Agitation, confusion, convulsion, dysarthria, emotional lability, speech disorder, thinking abnormal, vertigo
RESPIRATORY:Hiccup
The following infrequent adverse events were not seen with diazepam rectal gel but have been reported previously with diazepam use: depression, slurred speech, syncope, constipation, changes in libido, urinary retention, bradycardia, cardiovascular collapse, nystagmus, urticaria, neutropenia and jaundice.
Paradoxical reactions such as acute hyperexcited states, anxiety, hallucinations, increased muscle spasticity, insomnia, rage, sleep disturbances and stimulation have been reported with diazepam; should these occur, use of diazepam rectal gel should be discontinued.
To report SUSPECTED ADVERSE REACTIONS, contact Bausch Health US, LLC at 1-800-321-4576 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Drug Abuse and Dependence
Controlled Substance:DIASTAT contains diazepam, a Schedule IV controlled substance.
Abuse:DIASTAT is a benzodiazepine and a CNS depressant with a potential for abuse and addiction. Abuse is the intentional, non-therapeutic use of a drug, even once, for its desirable psychological or physiological effects. Misuse is the intentional use, for therapeutic purposes, of a drug by an individual in a way other than prescribed by a health care provider or for whom it was not prescribed. Drug addiction is a cluster of behavioral, cognitive, and physiological phenomena that may include a strong desire to take the drug, difficulties in controlling drug use (e.g., continuing drug use despite harmful consequences, giving a higher priority to drug use than other activities and obligations), and possible tolerance or physical dependence. Even taking benzodiazepines as prescribed may put patients at risk for abuse and misuse of their medication. Abuse and misuse of benzodiazepines may lead to addiction.
Abuse and misuse of benzodiazepines often (but not always) involve the use of doses greater than the maximum recommended dosage and commonly involve concomitant use of other medications, alcohol, and/or illicit substances, which is associated with an increased frequency of serious adverse outcomes, including respiratory depression, overdose, or death. Benzodiazepines are often sought by individuals who abuse drugs and other substances, and by individuals with addictive disorders (see WARNINGS, Abuse, Misuse, and Addiction).
The following adverse reactions have occurred with benzodiazepine abuse and/or misuse: abdominal pain, amnesia, anorexia, anxiety, aggression, ataxia, blurred vision, confusion, depression, disinhibition, disorientation, dizziness, euphoria, impaired concentration and memory, indigestion, irritability, muscle pain, slurred speech, tremors, and vertigo.
The following severe adverse reactions have occurred with benzodiazepine abuse and/or misuse: delirium, paranoia, suicidal ideation and behavior, seizures, coma, breathing difficulty, and death. Death is more often associated with polysubstance use (especially benzodiazepines with other CNS depressants such as opioids and alcohol).
Dependence:
Physical Dependence After Use of DIASTAT More Frequently Than Recommended
DIASTAT may produce physical dependence if used more frequently than recommended. Physical dependence is a state that develops as a result of physiological adaptation in response to repeated drug use, manifested by withdrawal signs and symptoms after abrupt discontinuation or a significant dose reduction of a drug. Although DIASTAT is indicated only for intermittent use (see INDICATIONS AND USAGEand DOSAGE AND ADMINISTRATION) ,if used more frequently than recommended, abrupt discontinuation or rapid dosage reduction or administration of flumazenil, a benzodiazepine antagonist, may precipitate acute withdrawal reactions, including seizures, which can be life-threatening. Patients at an increased risk of withdrawal adverse reactions after benzodiazepine discontinuation or rapid dosage reduction include those who take higher dosages (i.e., higher and/or more frequent doses) and those who have had longer durations of use (see WARNINGS, Dependence and Withdrawal Reactions) .
For patients using DIASTAT more frequently than recommended, to reduce the risk of withdrawal reactions, use a gradual taper to discontinue DIASTAT ( see WARNINGS, Dependence and Withdrawal Reactions) .
Acute Withdrawal Signs and Symptoms
Acute withdrawal signs and symptoms associated with benzodiazepines have included abnormal involuntary movements, anxiety, blurred vision, depersonalization, depression, derealization, dizziness, fatigue, gastrointestinal adverse reactions (e.g., nausea, vomiting, diarrhea, weight loss, decreased appetite), headache, hyperacusis, hypertension, irritability, insomnia, memory impairment, muscle pain and stiffness, panic attacks, photophobia, restlessness, tachycardia, and tremor. More severe acute withdrawal signs and symptoms, including life-threatening reactions, have included catatonia, convulsions, delirium tremens, depression, hallucinations, mania, psychosis, seizures, and suicidality.
Protracted Withdrawal Syndrome
Protracted withdrawal syndrome associated with benzodiazepines is characterized by anxiety, cognitive impairment, depression, insomnia, formication, motor symptoms (e.g., weakness, tremor, muscle twitches), paresthesia, and tinnitus that persists beyond 4 to 6 weeks after initial benzodiazepine withdrawal. Protracted withdrawal symptoms may last weeks to more than 12 months. As a result, there may be difficulty in differentiating withdrawal symptoms from potential re-emergence or continuation of symptoms for which the benzodiazepine was being used.
Tolerance
Tolerance to DIASTAT may develop after use more frequently than recommended. Tolerance is a physiological state characterized by a reduced response to a drug after repeated administration (i.e., a higher dose of a drug is required to produce the same effect that was once obtained at a lower dose). Tolerance to the therapeutic effect of benzodiazepines may develop; however, little tolerance develops to the amnestic reactions and other cognitive impairments caused by benzodiazepines.
Overdosage
Overdosage of benzodiazepines is characterized by central nervous system depression ranging from drowsiness to coma. In mild to moderate cases, symptoms can include drowsiness, confusion, dysarthria, lethargy, hypnotic state, diminished reflexes, ataxia, and hypotonia. Rarely, paradoxical or disinhibitory reactions (including agitation, irritability, impulsivity, violent behavior, confusion, restlessness, excitement, and talkativeness) may occur. In severe overdosage cases, patients may develop respiratory depression and coma. Overdosage of benzodiazepines in combination with other CNS depressants (including alcohol and opioids) may be fatal (see WARNINGS: Abuse, Misuse, and Addiction). Markedly abnormal (lowered or elevated) blood pressure, heart rate, or respiratory rate raise the concern that additional drugs and/or alcohol are involved in the overdosage.
In managing benzodiazepine overdosage, employ general supportive measures, including intravenous fluids and airway maintenance. Flumazenil, a specific benzodiazepine receptor antagonist indicated for the complete or partial reversal of the sedative effects of benzodiazepines in the management of benzodiazepine overdosage, can lead to withdrawal and adverse reactions, including seizures, particularly in the context of mixed overdosage with drugs that increase seizure risk (e.g., tricyclic and tetracyclic antidepressants) and in patients with long-term benzodiazepine use and physical dependency. The risk of withdrawal seizures with flumazenil use may be increased in patients with epilepsy. Flumazenil is contraindicated in patients who have received a benzodiazepine for control of a potentially life-threatening condition (e.g., status epilepticus). If the decision is made to use flumazenil, it should be used as an adjunct to, not as a substitute for, supportive management of benzodiazepine overdosage. See the flumazenil injection Prescribing Information.
Consider contacting the Poison Help line (1-800-221-2222) or a medical toxicologist for additional overdosage management recommendations.
Diastat Dosage and Administration
This section is intended primarily for the prescriber; however, the prescriber should also be aware of the dosing information and directions for use provided in the patient package insert.
A decision to prescribe diazepam rectal gel involves more than the diagnosis and the selection of the correct dose for the patient.
First, the prescriber must be convinced from historical reports and/or personal observations that the patient exhibits the characteristic identifiable seizure cluster that can be distinguished from the patient’s usual seizure activity by the caregiver who will be responsible for administering diazepam rectal gel.
Second, because diazepam rectal gel is only intended for adjunctive use, the prescriber must ensure that the patient is receiving an optimal regimen of standard anti-epileptic drug treatment and is, nevertheless, continuing to experience these characteristic episodes.
Third, because a non-health professional will be obliged to identify episodes suitable for treatment, make the decision to administer treatment upon that identification, administer the drug, monitor the patient, and assess the adequacy of the response to treatment, a major component of the prescribing process involves the necessary instruction of this individual.
Fourth, the prescriber and caregiver must have a common understanding of what is and is not an episode of seizures that is appropriate for treatment, the timing of administration in relation to the onset of the episode, the mechanics of administering the drug, how and what to observe following administration, and what would constitute an outcome requiring immediate and direct medical attention.
Calculating Prescribed Dose
The diazepam rectal gel dose should be individualized for maximum beneficial effect. The recommended dose of diazepam rectal gel is 0.2-0.5 mg/kg depending on age. See the dosing table for specific recommendations.
| Age (years) | Recommended Dose |
|---|---|
|
2 through 5 |
0.5 mg/kg |
|
6 through 11 |
0.3 mg/kg |
|
12 and older |
0.2 mg/kg |
Because diazepam rectal gel is provided as unit doses of 2.5, 5, 7.5, 10, 12.5, 15, 17.5, and 20 mg, the prescribed dose is obtained by rounding upward to the next available dose. The following table provides acceptable weight ranges for each dose and age category, such that patients will receive between 90% and 180% of the calculated recommended dose. The safety of this strategy has been established in clinical trials.
| 2 - 5 Years | 6 - 11 Years | 12+ Years | |||
|---|---|---|---|---|---|
| 0.5 mg/kg | 0.3 mg/kg | 0.2 mg/kg | |||
| Weight | Dose | Weight | Dose | Weight | Dose |
| (kg) | (mg) | (kg) | (mg) | (kg) | (mg) |
|
6 to 10 |
5 |
10 to 16 |
5 |
14 to 25 |
5 |
|
11 to 15 |
7.5 |
17 to 25 |
7.5 |
26 to 37 |
7.5 |
|
16 to 20 |
10 |
26 to 33 |
10 |
38 to 50 |
10 |
|
21 to 25 |
12.5 |
34 to 41 |
12.5 |
51 to 62 |
12.5 |
|
26 to 30 |
15 |
42 to 50 |
15 |
63 to 75 |
15 |
|
31 to 35 |
17.5 |
51 to 58 |
17.5 |
76 to 87 |
17.5 |
|
36 to 44 |
20 |
59 to 74 |
20 |
88 to 111 |
20 |
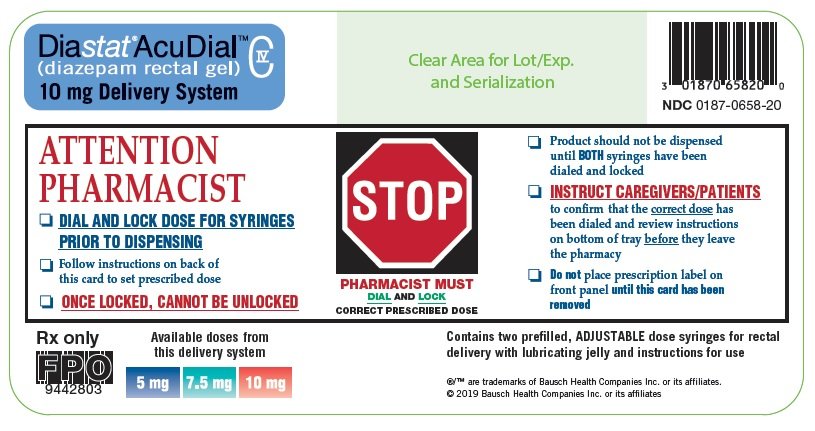
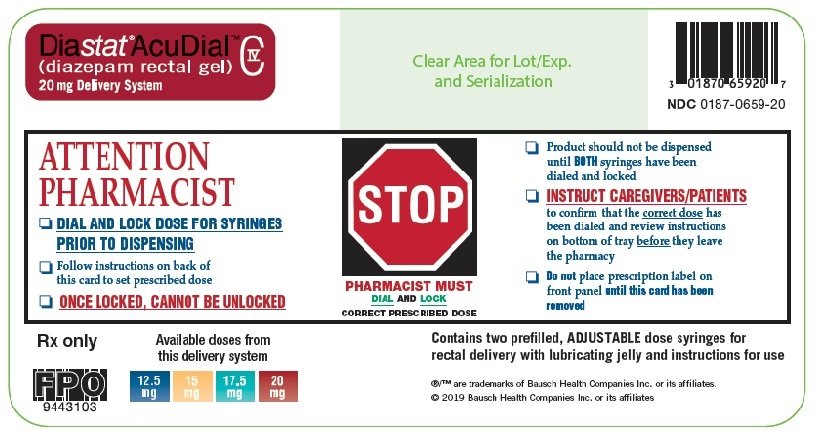
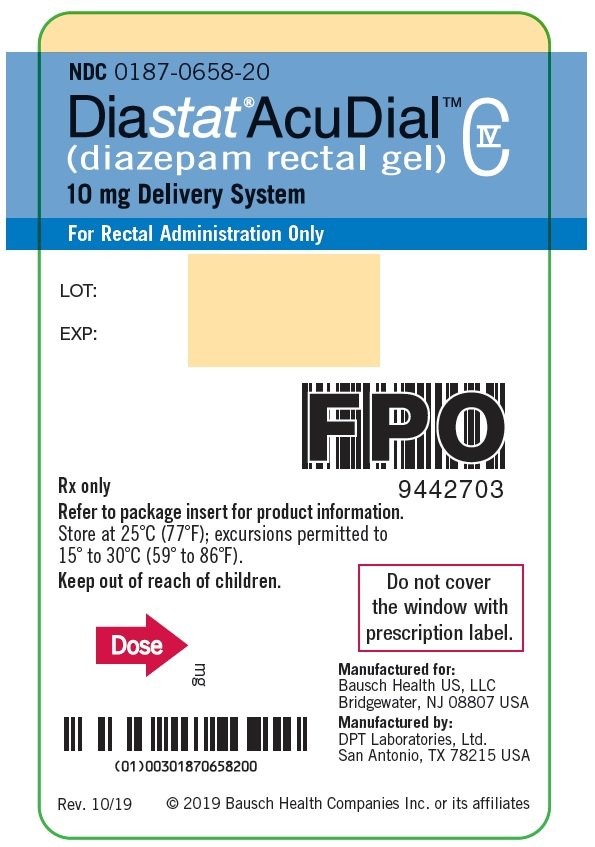
The rectal delivery system includes a plastic applicator with a flexible, molded tip available in two lengths. The DIASTAT ®ACUDIAL™ 10 mg syringe is available with a 4.4 cm tip and the DIASTAT ®ACUDIAL™ 20 mg syringe is available with a 6.0 cm tip. DIASTAT ®2.5 mg is also available with a 4.4 cm tip.
In elderly and debilitated patients, it is recommended that the dosage be adjusted downward to reduce the likelihood of ataxia or oversedation.
The prescribed dose of diazepam rectal gel should be adjusted by the physician periodically to reflect changes in the patient’s age or weight.
The DIASTAT ®2.5 mg dose may also be used as a partial replacement dose for patients who may expel a portion of the first dose.
Additional Dose
The prescriber may wish to prescribe a second dose of diazepam rectal gel. A second dose, when required, may be given 4-12 hours after the first dose.
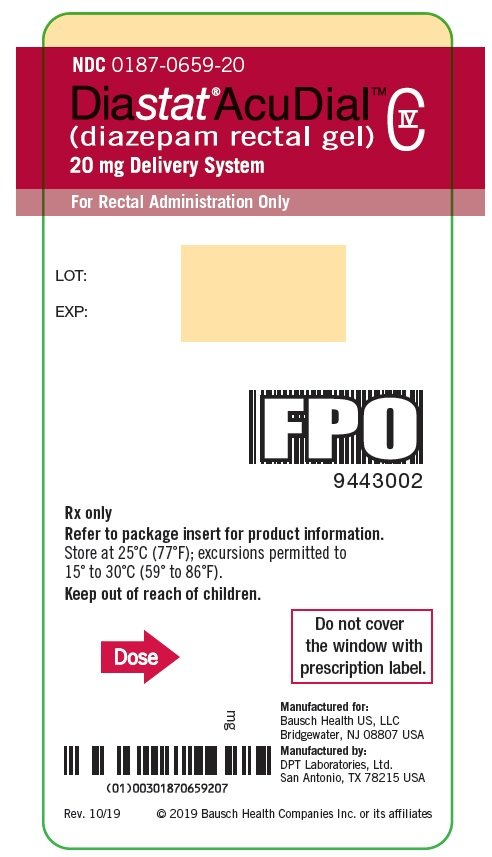
How is Diastat supplied
Diazepam rectal gel rectal delivery system is a non-sterile, prefilled, unit dose, rectal delivery system. The rectal delivery system includes a plastic applicator with a flexible, molded tip available in two lengths, designated for convenience as 10 mg Delivery System and 20 mg Delivery System. The available doses from 20 mg delivery system are 12.5 mg, 15 mg, 17.5 mg and 20 mg. The available doses from 10 mg delivery system are 5 mg, 7.5 mg and 10 mg. The diazepam rectal gel delivery system is available in the following three presentations:
|
DIASTAT® |
Rectal Tip Size |
NDC |
|
2.5 mg Twin Pack |
4.4 cm |
66490-650-20
|
|
DIASTAT®ACUDIAL™ |
Rectal Tip Size |
NDC |
|
10 mg Delivery System Twin Pack |
4.4 cm |
0187-0658-20 |
|
20 mg Delivery System Twin Pack |
6.0 cm |
0187-0659-20 |
Each Twin Pack contains two diazepam rectal gel delivery systems, two packets of lubricating jelly, and administration and disposal Instructions available on the bottom of the package. DIASTAT ACUDIAL is also packed with Instructions for Caregivers upon receipt from pharmacy.
Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F) [see USP Controlled Room Temperature].
DIASTAT
®ACUDIAL™
INSTRUCTIONS FOR CAREGIVERS
UPON RECEIPTFROM PHARMACY
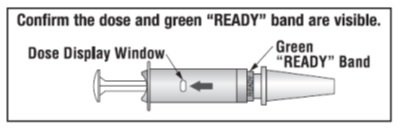
- Remove the syringe from the case.
- Confirm the dose prescribed by your doctor is visible and if known, is correct.
FOR EACH SYRINGE:
- Confirm that the prescribed dose is visible in the dose display window.
- Confirm that the green “READY” band is visible.
- Return the syringe to the case.
SEE PHARMACIST IF YOU HAVE ANY QUESTIONS ABOUT THESE INSTRUCTIONS.
The Instructions are also available on the bottom of each drug product package.
CAUTION: Federal law prohibits the transfer of this drug to any person other than the patient for whom it was prescribed.
Distributed by:
Bausch Health US, LLC
Bridgewater, NJ 08807 USA
Manufactured by:
DPT Laboratories, Ltd.
San Antonio, TX 78215 USA
®/™ are trademarks of Bausch Health Companies Inc. or its affiliates.
© 2023 Bausch Health Companies Inc. or its affiliates
9435005 Rev. 7/2023
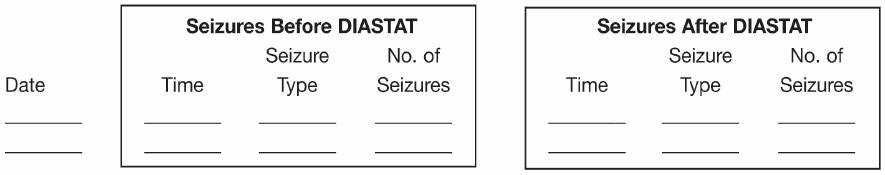
IMPORTANT
Read first before using
To the caregiver using DIASTAT ®:
Please do not give DIASTAT ®until:
- You have thoroughly read these instructions
- Reviewed administration steps with the doctor
- Understand the directions
To the caregiver using DIASTAT®ACUDIAL™:
Please do not give DIASTAT®ACUDIAL™until:
- You have confirmed:
- • Prescribed dose is visible and if known, is correct
- • green “READY” band is visible
- You have thoroughly read these instructions
- Reviewed administration steps with the doctor
- Understand the directions
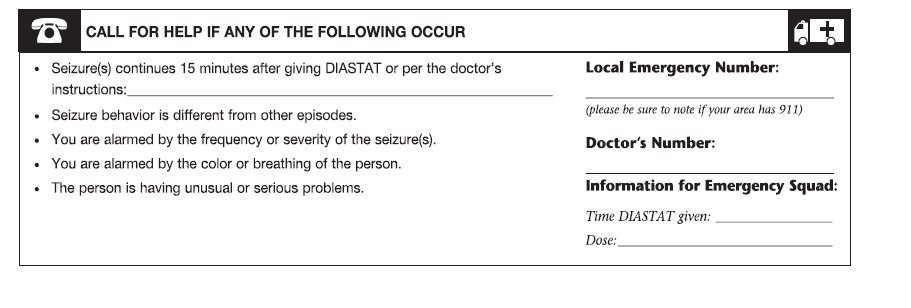
Please do not administer DIASTAT until you feel comfortable with how to use DIASTAT. The doctor will tell you exactly when to use DIASTAT. When you use DIASTAT correctly and safely you will help bring seizures under control. Be sure to discuss every aspect of your role with the doctor. If you are not comfortable, then discuss your role with the doctor again.
To help the person with seizures:
✓ You must be able to tell the difference between cluster and ordinary seizures.
✓ You must be comfortable and satisfied that you are able to give DIASTAT.
✓ You need to agree with the doctor on the exact conditions when to treat with DIASTAT.
✓ You must know how and for how long you should check the person after giving DIASTAT.
To know what responses to expect:
✓ You need to know how soon seizures should stop or decrease in frequency after giving DIASTAT.
✓ You need to know what you should do if the seizures do not stop or there is a change in the person’s breathing, behavior or condition that alarms you.
If you have any questions or feel unsure about using the treatment, CALL THE DOCTORbefore using DIASTAT.
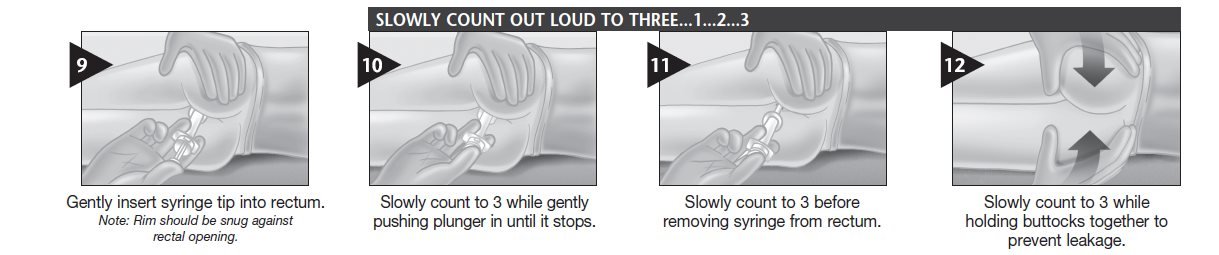
When to treat.Based on the doctor’s directions or prescription.Your doctor may prescribe a second dose of diazepam rectal gel. If a second dose is needed, give it 4 hours to 12 hours after the first dose.
____________________________________________________________________________________
____________________________________________________________________________________
Special considerations.
DIASTAT should be used with caution:
- In people with respiratory (breathing) difficulties (e.g., asthma or pneumonia)
- In the elderly
- In women of child bearing potential, pregnancy and nursing mothers
Discuss beforehand with the doctor any additional steps you may need to take if there is leakage of DIASTAT or a bowel movement.
Patient’s DIASTAT dosage is:__________mg
Patient’s resting breathing rate _________ Patient’s current weight ____________
Confirm current weight is still the same as when DIASTAT was prescribed ____________
Check expiration date and always remove cap before using. Be sure seal pin is removed with the cap.
TREATMENT 1
------------------------------------------------------------------------------------------------------------------------------
Important things to tell the doctor:
Things to do after treatment with DIASTAT:
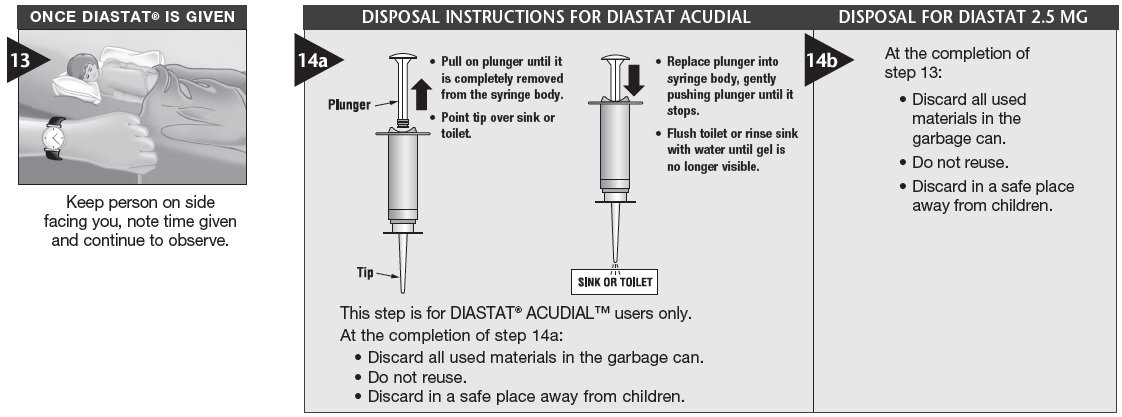
Stay with the person for 4 hours and make notes on the following:
- Changes in resting breathing rate_______________________________________________________
- Changes in color ___________________________________________________________________
- Possible side effects from treatment_____________________________________________________
- Your doctor may prescribe a second dose of diazepam rectal gel. If a second dose is needed, give it 4 hours to 12 hours after the first dose.
TREATMENT 2
------------------------------------------------------------------------------------------------------------------------------
Important things to tell the doctor:
Things to do after treatment with DIASTAT:
Stay with the person for 4 hours and make notes on the following:
- Changes in resting breathing rate_______________________________________________________
- Changes in color ___________________________________________________________________
- Possible side effects from treatment_____________________________________________________
Distributed by:
Bausch Health US, LLC
Bridgewater, NJ 08807 USA
Manufactured by:
DPT Laboratories, Ltd.
San Antonio, TX 78215 USA
®/™ are trademarks of Bausch Health Companies Inc. or its affiliates.
© 2023 Bausch Health Companies Inc. or its affiliates
9435005 Rev. 7/2023
| DIASTAT
diazepam gel |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| DIASTAT
diazepam gel |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| Labeler - Bausch Health US, LLC (831922468) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| DPT Laboratories, Ltd. | 832224526 | manufacture(0187-0658, 0187-0659) | |
More about Diastat (diazepam)
- Check interactions
- Compare alternatives
- Reviews (2)
- Latest FDA alerts (2)
- Side effects
- Dosage information
- During pregnancy
- Drug class: benzodiazepine anticonvulsants
- Breastfeeding